Don’t let pelvic girdle pain limit your activities.
Many of us love to get out and enjoy our wonderful Alaskan outdoors. However for some pelvic pain can limit our ability to do the things we love.
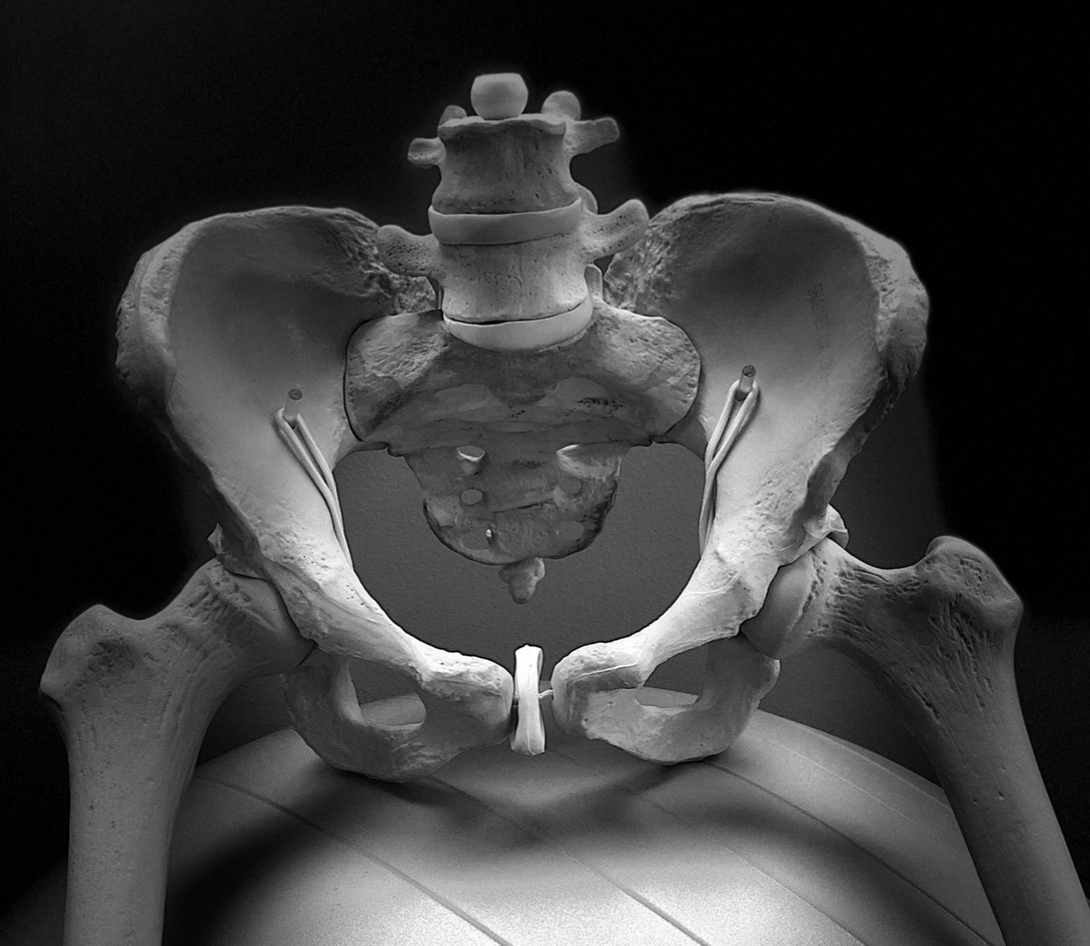
What is pelvic girdle pain?
Misalignment during pregnancy can cause pain in the front or back of the pelvis (symphysis pubis and sacroiliac or SI joints), the low back, hips, legs, and even in the pelvic floor. This can be anywhere from mild and annoying to completely debilitating.
It is relatively common but not normal. Contrary to myth, women do not need to suffer or wait until they have their baby, to get relief.
Activities that can be painful include walking, stairs, turning in bed, or getting in or out of a car or chair.
Who gets pelvic girdle pain?
About 20% of pregnant women experience pelvic girdle pain. It can persist for more than 3 months after delivery and occasionally much longer. Research has found that the degree of asymmetry between the right and left sides of the pelvis is a factor.
What can I do about it?
Avoid stretching. Stability, not flexibility, is key.
Wear good shoes. Athletic shoes with good stability can be helpful.
Avoid standing on one leg to get dressed, try sitting to pull each pant leg on.
Get in and out of the car (or bed) with your legs together as if you were wearing an imaginary pencil skirt.
Sleep with a pillow between your legs.
Squeeze the pillow gently before turning in bed.
Try going up the stairs sideways.
Don’t carry a heavy bag on one side, use a bag pack or cross body bag.
During intercourse, use positions where your legs stay together.
Avoid heavy lifting.
Modify your activity, for example, limit walking or standing time to less than 20 minutes at a time.
When should you get help?
If you notice pain in the front or back of your pelvis, hips, back, into your leg(s) or pelvic floor during pregnancy or postpartum, mention it to your health care provider. They may recommend seeing a physical therapist. Alternatively, you can contact a women’s health physical therapy specialist (also known as a pelvic health specialist) for more information.
Your physical therapist will teach you specific exercises for your pelvic pattern.
They will also show you behavioral changes to keep it from happening again, for example how to position yourself during sleep, sitting, standing and sit to stand.
Additional resources.
Physical therapists that specialize in women’s health have advanced training in this area. Just a few appointments can be enough to learn precisely which exercises you can do on your own to stabilize your pelvis and relieve pain.
To find a women’s health physical therapist near you go to: https://www.womenshealthapta.org.
Do I need a referral for Physical Therapy?
In Alaska, physical therapists have what is known as ‘direct access’ which means that patients can legally see them directly, without a referral. A few health insurances do require a prescription.
What other problems do women’s health physical therapists see?
Urinary incontinence: It is not normal to leak when you laugh, cough or even jump. The latest approaches include treating the body as a whole system, not solely doing kegels.
Pelvic organ prolapse: When the muscles that hold up the pelvic organs get weak or overstretched they can drop from their normal position. A common symptom is pressure in the pelvic floor. Talk to your medical provider if you have symptoms.
Separation of the abdominal muscles (diastasis recti): Physical therapists are uniquely qualified to assess and treat this condition. They will also be able to give you an exercise program and tell you what activities you should and shouldn’t do, or when to get back to running/sports.
Other types of pelvic pain: For example; painful intercourse, vaginismus and vulvodynia. There are many possible causes so make sure you talk to your healthcare provider. They may recommend you see a women’s health physical therapist.